Fighting Fluid Retention on Peritoneal Dialysis Vol 1: Climbing Negative UF

Hello There!
Over the course of June 2023, every morning, I began to notice rising negative UF (ultrafiltration) figures on my Baxter Claria machine which ultimately led to me becoming partially overloaded with fluid and instigated a Dialysis prescription change by my nephrologist. Despite having been on dialysis for over 2 years and finally hitting the balance in work, life and dialysis. I was really taken aback by this regime change and felt compelled to document what feels like another very uncertain and emotional time in my journey with kidney disease, kidney failure and dialysis.
I hope this series brings some peace to others who are also going through similar issues of: fluid retention, fluid overload, and dialysis prescription change.
June 2023: The Hottest Summer Heatwave in UK
This year, we experienced some of the hottest weather ever recorded in the UK and the beginning of that heatwave was in June. For those who are on dialysis, are burdened with the knowledge that hot weather does not bode well for those on dialysis because of the fluid restrictions we are prescribed. Personally, I have been advised to not exceed 1L of fluid a day, particularly as I no longer pass urine and wholly rely on the machine to remove excess fluid from my body.
Hence, you can imagine the beating sun rays even through the windows and walls of my house did not help with my health outcomes. During the month of June, I was recording increasing Blood Pressure results each morning and night as well as increasing negative UF on my morning Baxter screen. Ultimately, by the end of the month, I was looking more swollen and fluid overloaded than ever before.
What does it feel like to be Fluid Overloaded as a PD Patient?
As a young person on PD, I feel like we do not present fluid overload or fluid retention like our older counterparts. A young person can sinisterly mask their fluid retention all over their body such as their back and limbs which can disguise the overall effect as increased flesh weight and is not as noticeable or alarming as ballooning feet, hands or ankles as typically presented in adults. This can make it more difficult to identify the effects of fluid retention!
I personally held a lot of fluid on my face rather than my feet and ankles, which is where it is typically seen. I later found out that not only was I carrying fluid on my face but my entire body: shoulders, chest, back, arms and legs! The general spread of fluid retention around the body is likely because I perform my dialysis lying down, allowing the fluid to travel everywhere.
I did scarily once notice that when looking in the mirror one morning, physically watch the fluid drain from my face to another more secret hiding place. Spooky!
How To Tell if I am Fluid Overloaded as a PD Patient?
There are 2 ways for a PD Patient to tell if they are fluid overloaded from home:
1. Looking in the Mirror
This is looking at your overall features and silhouette. Do you see an increased plumpness? Remember fluid retention will look like you have seemingly gained a noticeable amount of weight in a matter of days! Albeit I doubt anyone is gaining weight on the renal diet!
2. Daily Weigh-in Morning and Night
The most accurate is to check your weight before connecting to dialysis and after everyday and notice any significant fluctuations of +/- 2Kgs. Remembering that any extraneal (day fills) you may have in your stomach during the day will contribute to your weight (1000ml = 1kg). So a fluctuation in excess of that is likely fluid retention!
3. Unexplained high blood pressure (indicator)
The increased fluid retention on your body can increase your blood pressure despite perhaps not changing anything in your routine: your medication, your diet and exercise plan.
For me, it was the unexplained high blood pressure that triggered the alarms for me that something was wrong and was what I presented to my Nephrologist when I next saw him. In all honesty, I barely registered the fluid overload even though I did experience changes in my physique and face structure and towards the end of the month was experiencing finger and ankle joint pain. However, it was easy for me to dismiss these over time as they were only noticeable in the mornings and would dissipate later in the day. It is crazy what we get used to over time! Don’t ignore what your body is telling you! I was too ready to ignore the signs to enjoy the lovely sunshine of summer.
Furthermore, since starting dialysis, I have become particularly adverse to looking at myself in the mirror. When I first returned home, I looked really rough and the bulging stomach from PD and blooming acne from renal failure just wasn’t something I was ready to face everyday and became a steady habit to avoid looking in the mirror. For similar reasons, I stopped weighing myself about a month after returning home, once my PD had settled. This allowed me to miss all the physical signs!
As someone who had been on PD for 2 years with relatively few issues, I had in short become complacent.
What Causes Fluid Overload / Fluid Retention in Peritoneal Dialysis Patients?
Fluid retention largely appears when there are reportedly Negative Ultrafiltration Figures on your Baxter machine in the morning after dialysis. This means that more fluid stayed on your body than was expelled through dialysis in the last drain. This remaining fluid is then reabsorbed into the body and swells your body. Too much in excess leads to Fluid Overload which can lead to quite fatal symptoms I am told by my doctor: high BP (Heart Attack) and Breathing issues (pulmonary edema). Both of which we should try to avoid!
What causes Negative UF for Peritoneal Dialysis Patients?
My understanding is that the following can cause Negative UF:
- Dehydration
Solution: Drink more during the day / on dialysis - Insufficient Bowel Movement
Solution: Take your laxatives [Guilty] - Fibrin blocking the Catheter holes within your stomach
Inspect: Drain Bags for cotton like floating strands of fibrin particularly in any painful drains.
Solution: If not resolved by itself, inform the nurse and they will provide special medicine to help break up the fibrin. - Incorrect position of the Catheter.
Solution: Sitting upright during drain cycles or moving side to side during drain to stimulate the catheter.
Solution: Consult with nephrologist, may result in a procedure to surgically move the catheter into a more desirable position - Peritonitis 😥
Inspect: Drain bags for cloudiness or particles
Solution: Inform your Nurses and get yourself on antibiotics ASAP.
Generally, 2 things that I skipped over in my dialysis care: (1) my laxatives and (2) performing a daily weigh in. I have since rectified it! But, the lack of weigh-ins meant my medical team could not monitor that my weight was steadily increasing due to fluid retention and my wilful dislike of taking my Lactulose meant that I was not passing as much as I needed! A full bowel is never good for PD! This combination had led to steady rise in my fluid retention and generally more painful dialysis sessions and the hot weather did not help either! I was either consuming too much water in the day or was devastatingly dehydrated and too dry to pass a bowel movement. Just can’t win!
I now perform my weigh-ins and take both my senna and lactulose everyday. I particularly drink a glass of water with my lactulose so that there is something for the medicine to draw down into my bowels to make me pass.
Speaking to my Nephrologist: Changing my Dialysis Prescription
I met with my Nephrologist at the start of July 2023, coming to him with problems climbing negative UF and high BP readings of 160+/100+ despite not having changed my medication, diet or exercise.
Once illuminated about my bad behaviour for not weighing myself nor taking my laxatives leading to a steady build up of fluid, I was told that I had to change dialysis prescription:
Old prescription
2x 5000ml 1.36% Dianeal (Yellow)
1x 2000ml Extraneal (Purple) but only 1000ml day fill
4 Cycles for 9 Hours
New Prescription
1x 5000ml 2.26% Dianeal (Green) on the heater
2x 5000ml 1.36% Dianeal (Yellow)
1x 2000ml Extraneal (Purple) with an increased to 1200ml fill
5 Cycles for 9 Hours
To be honest, I was feeling really mournful over the change and was only given a shed of optimism that my nephrologist said it would only be temporarily for a couple weeks and we would revisit returning to my old regime soon. Additionally, to tie me over, I was prescribed even more blood pressure meds to dampen my rising BP until I had my fluid retention and dialysis under control.
And so began another hill to climb on this Dialysis Journey!
Tune in next week for Fighting Fluid Retention on Peritoneal Dialysis Vol 2: Weight Loss on Dialysis Prescription Change
A Little About Me:
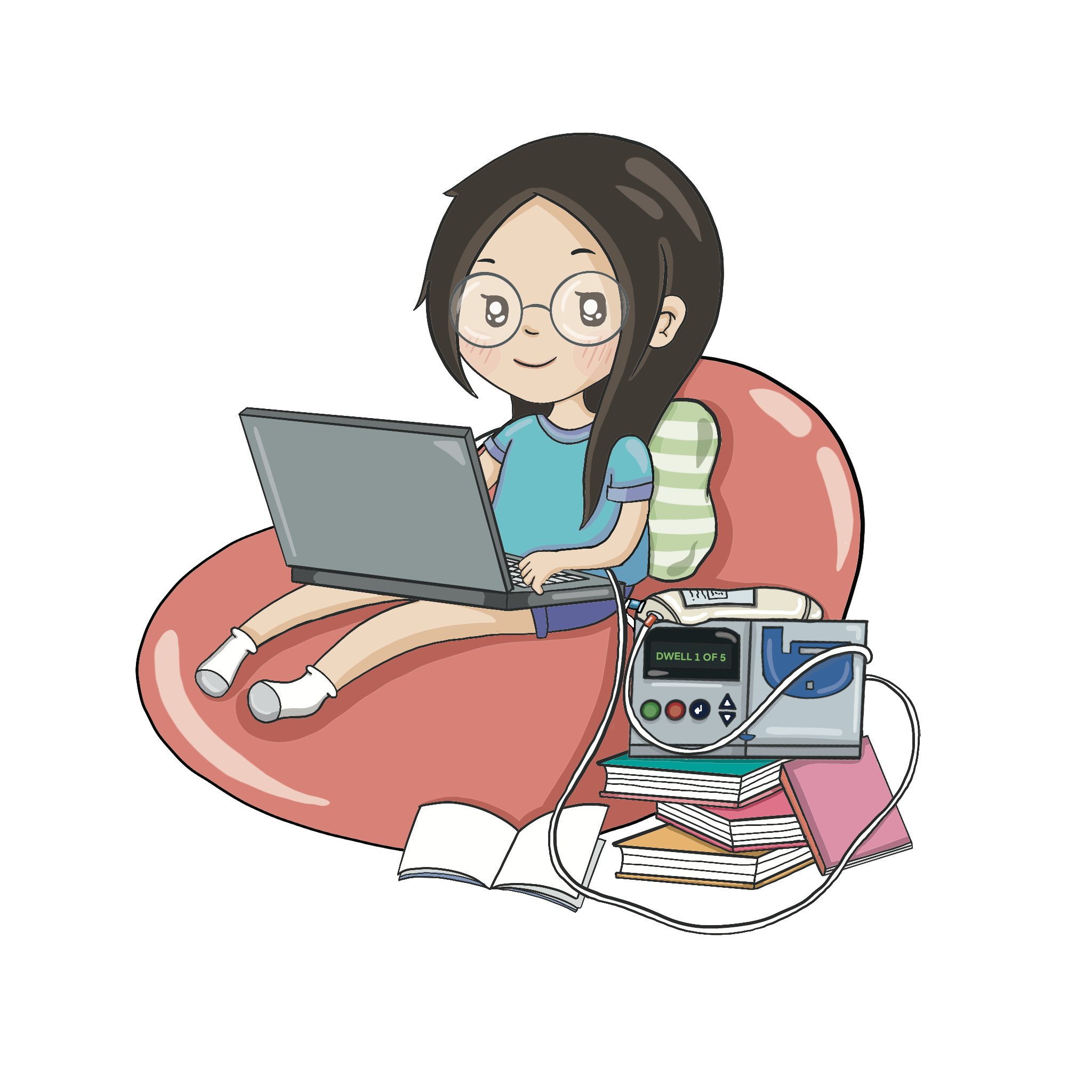
My name is Lai and I am 26 years old living on Home Peritoneal Dialysis in the UK. I started home peritoneal dialysis in the height of the pandemic in the winter of 2020 and have been on daily 9 hour overnight dialysis ever since, whilst waiting on the national transplant list. I live with my two parents at home but I am the one with the sole responsibility of setting up and dismantling my machine and the general monitoring of my day to day health.
Follow me on:
IG: @My_Kidney_and_Lai
YT: My Kidney and Lai
Working on how to add comments to my blog posts, feel free to reach out to me on my Instagram DMs in the meantime!